Coronavirus – bioengineering for testing COVID-19
- MCS

- Mar 11, 2020
- 9 min read
Updated: Mar 25, 2020
In my last post I mentioned viruses, and how they shape all living forms in the World. Sadly, this time I have to post again about viruses mostly because of the current pandemic caused by COVID-19 or more properly named the virus SARS-CoV-2. Yes.. pandemic, the U.S. just hit 1000 cases, this trend keeps growing exponentially in the U.S and other countries as well. As pointed out by Bill Gates in The New England Journal of Medicine, this pandemic can especially affect low- and middle-income countries overwhelming their health systems (1). Therefore, a practical methodology for extensive testing would be helpful for all countries. For starters, I am not a physician, not a virologist, not an immunologist, not even a microbiologist; I am a bio-engineer that is hopeful in making a difference. This time I investigated examples of bioengineering techniques for detecting COVID-19. I will focus on three approaches that could be adopted for research institutes, and others, outside the clinics, for detecting COVID-19 and contribute to decrease the burden that thousands of tests might cause in specialized personnel from the hospitals.
Scientists and engineers from all disciplines (even outside the biological sciences) must contribute with some adventurous thoughts, specialized techniques, fast detection methods, etc., maybe some might actually be useful for people in the front-line fighting this global disease.
General info about the current outbreak:
I won’t repeat all information that it’s been coming up online because it’s easily available and it is constantly updating. I will provide some websites:
The Centers for Diseases Control (CDC) website: https://www.cdc.gov/coronavirus/2019-ncov/index.html has relevant info regarding the following points: 1) How it spreads, 2) symptoms, 3) prevention, 4)testing, 5)traveling, and 6) laboratories resources such as requests for diagnostic tools (RT-PCR kit or COVID-19 in cell culture).
This is an interview with Dr. Akiko Iwasaki, a highly recognized immunologist, and one of my favorite scientists, here she answers general questions that are VERY USEFUL to all of us.
You could get the actual cases worldwide, news by country, estimated transmission and fatality rates, estimated incubation period from here: https://www.worldometers.info/coronavirus/ or here: https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
A list of different vaccines and therapies against COVID-19 are under development and can be found here: https://www.biocentury.com/article/304515
DIAGNOSTICS is a big world that can prevent so many cases in all countries, COVID-19 can give mild symptoms(2), and can silently spread this is why it’s important to be cautious and implement self-isolation procedures if you are able to, maybe you will be fine but older people won’t.
OK. enough with the general info.
At this point, is not how many people have recovered and how many have died. It's
why did this outbreak happen? how is it spreading all over the World? how are we as society behaving? how are we prepared for the next outbreak (or for the current one)?. Too many questions unanswered, but one is specially intriguing for me: What can bioengineering offer to mitigate this outbreak?.
Bioengineering can offer many approaches for 1) monitoring existing diseases and also for 2) developing therapeutics, and the science behind them.
For this post, I will focus on the testing of COVID-19 with bioengineering approaches. Diagnostics can really slow down the spreading of this new virus. This is the most effective way in terms of buying some time for the patient so it can be adequately treated, and for other people and governments so they can implement aggressive safety guidelines that can hopefully prevent further spreading. I think that we are in this stage where diagnostics is so critical, and depending on how well it is executed, and how well-informed our society becomes, the outcome of the epidemic can dramatically change in your location. In fact, location is always crucial in the severity of a disease. The morbidity of a disease impacts countries with a deficient healthcare system (not necessarily from low-income countries), lack of healthcare facilities, and low-income isolated communities. Morbidity can be mitigated with efficient testing procedures. Consequently, a fast, cheap, and portable device should always be the priority of bioengineers dedicated to diagnostics. This idea has been around in the scientific community for a while now and its often times referred as point of care (POCs) diagnostics devices. The WHO stated that an ideal POC test should comply with the ASSURED (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free and Deliverable to end users) criteria. Of course, this takes some time, but a general bio-engineered platform that can be coupled with a different target (such as COVID-19) and comply with the ASSURED criteria will be essential for this and future pandemics.

Figure 1. Radiography and CT scan of an infected person with COVID-19. A) Radiography of 1-week infected lungs. B) Chest CT images of a patient with fever for 11 days. Both images A and B were adapted from Zhe Xu et al., (2020)(3) and Tao Ai et al., (2020)(4), respectively. Patchy shadows shown in A) and ground-glass opacities in B) can be observed as the disease progresses. These shown shadows or patterns cause the shortness of breath, typical general symptom of COVID-19.
Currently, hospitals and other institutions in the front-line of battle first look at the symptoms such as cough, chills, fever, fatigue and short of breath, then they employ chest x-ray and take a look at the lungs for examining them at a macroscopic level as shown in Figure 1A or they perform a more detailed study called chest computed tomography (CT) which can produce slices (detailed pictures) of the lung (Figure 1B). In addition, they could analyze tons of parameters such as counting of leukocytes (e.g., lymphocytes, monocytes, eosinophils, basophils and neutrophils), which are the specialized type of cells in your immune system that normally go up during infection. For COVID-19, lymphopenia, or the low count of lymphocytes, is a common feature of the patients (3). This was also observed for SARS-CoV when the virus infected immune cells and disseminated to other organs. However, it's too early to draw conclusions about cell-level pathogenesis of COVID-19. What society needs is fast and accurate testing procedures to stop further contagion.
What can bioengineering offer to detect this EXISTING NEW outbreak?
I consider these techniques worth talking about because of their potential for large-scale applicability. These are examples of bioengineering providing some answers to a pressing issue like this.
The first presented technique is not a pure bioengineering approach, it combines CT scans with machine learning. This methodology has the potential for massive diagnostics of COVID-19. Usually, the physician takes a look at these slices and analyzes patterns that are common of the pathology of COVID-19. These patterns instead of being individually analyzed, they can feed an algorithm (a program) so it can process hundreds, thousands or millions of images very rapidly and identify potential patients with COVID-19 based on the pattern of their CT scans. In fact, the analyses of the CT scans were reported to be correlated with the gold-standard RT-PCR which reinforces the applicability of CT scans for COVID-19 diagnostics and increases the confidence of employing deep learning algorithms for processing these images. This model called DeepPneumonia, as other deep learning algorithms, had the training, validation, and test data, and K-scores were extracted utilizing a convoluted neural network. The normalized predicted scores for the extracted details of each slice of the CT scan were above 0.8 (in a scale 0 to 1) (Figure 2). This model was experimentally validated with 88 COVID-19 patients and 86 healthy persons (5).

Figure 2. Extracted details from CT scans with normalized predicted scores. The red boxes indicate the extracted identified pattern, and the scores are a metric for the model. The maximum score is 1.00. This image was taken from the original study reported by Song Ying et al., (2020)(5).
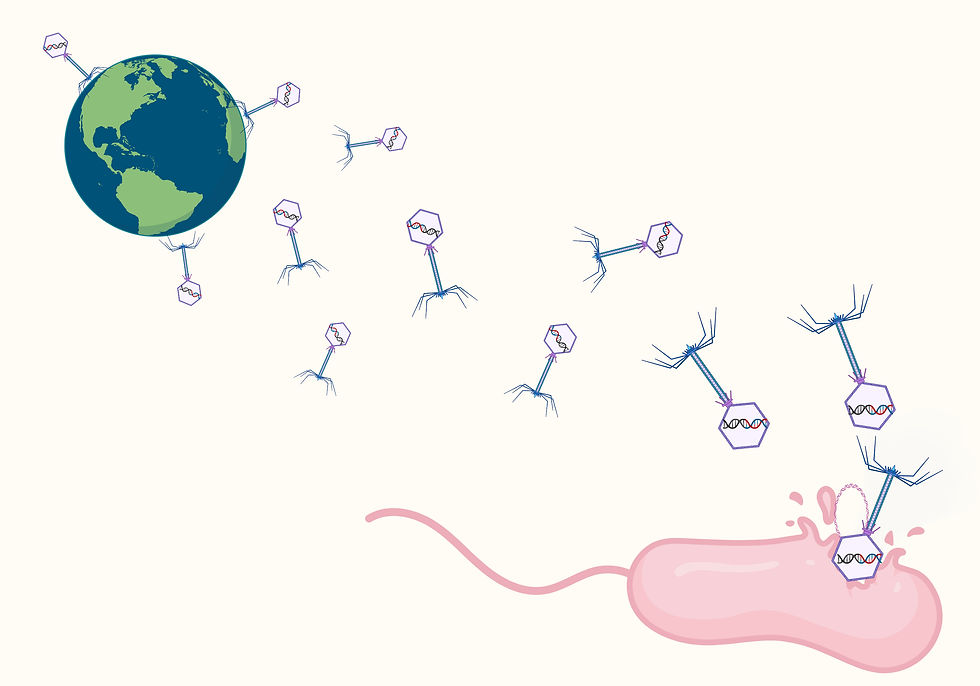
The fast paced of different research groups around the globe has also produced some new data about the elements of COVID-19 and the way it interacts with the host. The genome of this virus is known, the crystal structure of the main protease has been elucidated, and host (human) receptors (e.g., ACE2) are starting to be identified (Figure 3).

Figure 3.- Coronavirus COVID-19 structure. A) Morphology of COVID-19. B) Genomic organization. Identified proteins are shown, including the protein that binds ACE2 host receptor.
Even though the amount of knowledge about COVID-19 is limited, this is enough for applying bioengineering techniques for detection. As indicated by the CDC, specialized personnel can utilize a swab, collect sample of saliva, and perform reverse real-time PCR (Figure 4). However, the techniques presented in this post can be very useful in case of a massive demand of testing (which it should be the case), and also for testing in remote places (which it also should be the case).

Figure 4.- RT-PCR for detecting COVID-19. This is the official gold standard technique for testing and detection. Viral mRNA is extracted, then 1) primers, 2) probe with quencher, and 3) the reverse transcriptase are added to the viral mRNA. The different elements will bind to the RNA strand and the reverse transcriptase will produce cDNA (double strand DNA complementary to the original single strand mRNA from the virus). The polymerization also will break the quencher of the probe which will emit fluorescence. The amount of fluorescence is proportional to the amount of produced cDNA or initial viral mRNA. The RT-PCR typically involve several cycles with different temperatures therefore a machine called thermocycler is required.
Bioengineering offers another rapid approach for detecting COVID-19, this methodology can be applied in isolated regions because of its portability. This second approach is a derivative of the conventional RT-PCR. RT-LAMP or Loop-mediated isothermal amplification overcomes the thermocycler (the PCR machine) required for RT-PCR, it operates at one single temperature therefore a simple water batch or even room temperature conditions can do the job in as little as 5-10 minutes. This method can be coupled to inexpensive platforms such as paper and the color can be visible by the naked eye because of the action of pH indicator-based colorimetric assays which detect the amplification. RT-LAMP can be coupled to a microfluidic device (so it can be portable). A smartphone can be used to quantify the signal of detection and produce a YES or NO detection method. This technology was previously demonstrated to detect specifically ZIKA virus(6). This detection method is very versatile because by using a different set of primers, it could be used to detect other viruses. COVID-19 was reported to be detected using RT-LAMP (Figure 5). The authors reported a limit of detection of 10 copies of SARS-CoV-2, after the amplification of the ORF1ab gene (most diluted sample from Figure 5). The detection was possible within 10 – 40 minutes(7).

Figure 5. RT-LAMP diagnostic platform or iLACO detected COVID-19 by the naked eye. The most diluted solution (number 1) contained 10 copies of a specific COVID-19 gene and was enough to be visible. This figure was taken from original report from Lin Yu, et al., (2020) (7).
The third approach is a CRISPR-based technology that can detect trace amounts of COVID-19 RNA. Its name is Specific High Sensitivity Enzymatic Reporter UnLOCKing (SHERLOCK). Omar Abudayyeh, Jonathan S. Gootenberg and Feng Zhang published this technology in 2017 (8). SHERLOCK, similarly, to RT-LAMP, performs an isothermal amplification of the COVID-19 S and Orf1ab genes. Instead of having a probe with a quencher, the amplified material also contain reporters that can be cleaved by the Cas13a. The frequency of cuts will be proportional to the detection of a single molecule of viral RNA. This enzyme is the main difference with the classical CRISPR-Cas9 and is the key for detecting specific viral RNA. This video shows how Cas13a can detect viral RNA being this the principle of SHERLOCK.
After the reaction is completed, a dipstick can be placed in each reaction tube. This will produce a lateral flow read out with one control and one detection band (Figure 6).

Figure 6.- COVID-19 genes detected with SHERLOCK by lateral flow read out strip. The control band has to appear all the time for the reliability of the assay. The detection band will indicate a positive case of COVID-19 from a sample. The samples can be similar to the swabs utilized for RT-PCR. This image was taken from the original reported protocol available online here https://www.broadinstitute.org/files/publications/special/COVID-19%20detection%20(updated).pdf
Testing is the key for starting to contain the virus. These approaches for detecting COVID-19 are great possibilities for complementing the official RT-PCR test.
Please, follow the recommended procedures and stay COVID-19 free.
References
1. B. Gates, New engla nd journal, 1–3 (2020).
2. B. Zhou, F. Author, J. She Yadan Wang Xiancang Ma, The Lancet The Clinical Characteristics of Myocardial injury in Severe and Very Severe Patients with 2019 Novel Coronavirus Disease (2020) (available at https://ssrn.com/abstract=3539668).
3. Z. Xu et al., Case Report Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. 2600, 19–21 (2020).
4. T. Ai et al., Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2019, 200642 (2020).
5. Y. Song et al., Deep learning Enables Accurate Diagnosis of Novel Coronavirus (COVID-19) with CT images. medRxiv (2020), doi:10.1101/2020.02.23.20026930.
6. K. Kaarj, P. Akarapipad, J. Y. Yoon, Simpler, Faster, and Sensitive Zika Virus Assay Using Smartphone Detection of Loop-mediated Isothermal Amplification on Paper Microfluidic Chips. Sci. Rep. 8 (2018), doi:10.1038/s41598-018-30797-9.
7. L. Yu et al., medRxiv, in press, doi:10.1101/2020.02.20.20025874.
8. J. S. Gootenberg et al., Nucleic acid detection with CRISPR-Cas13a/C2c2. Science (80-. ). 356, 438–442 (2017).


Comments